Review: Role of Point-of-Care Ultrasound During the COVID-19 Pandemic: Our Recommendations in the Management of Dialytic Patients
Source: Ultrasound J (2020) 12:30
Introduction
The COVID-19 pandemic that the world is facing leads to extremely high number of infected patients, and to a surge that is creating a serious crisis even in the most advanced medical organizations. The big challenge is to efficiently and quickly recognize patients with COVID-19 pneumonia who need isolation, hospitalization and intensive care management.
The special role of lung ultrasound during the COVID‑19 pandemic
Lung ultrasound (LUS) has been well validated in the evaluation of several respiratory conditions. LUS is an image method that classically allows the evaluation of the pulmonary periphery which makes it an excellent technique in the assessment of COVID-19. This is because the lesions observed in CT scan of patients with COVID-19 are generally peripheral and subpleural. LUS is also advantageous in the management of patients with COVID-19 since the treating physician can perform LUS at the bedside, obtain and interpreted the images.
Basic principles of LUS
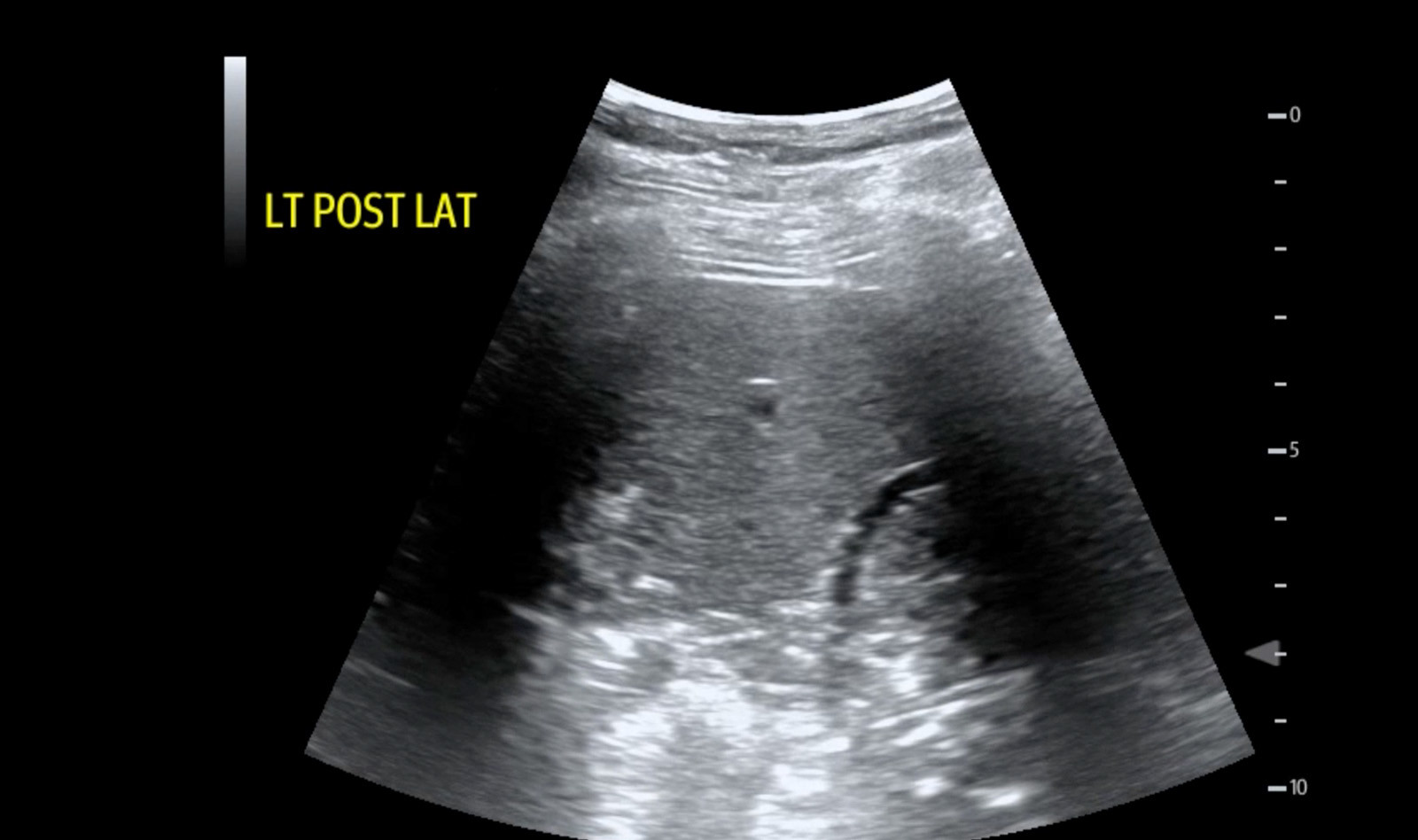
LUS images are most often not anatomical like in other ultrasound fields. Rather, they are based on artifacts generated by the interaction of the ultrasound beam with the acoustic interface between the chest wall tissue and air in the alveoli distributed in the pulmonary surface. Therefore, LUS is the study of lung diseases that abut the pleura.
Lung patterns
In a normal lung with air filling the alveoli, the ultrasound beam is completely reflected back to the transducer due to the high acoustic impedance between the chest wall tissue and air in the alveoli. This creates a “normal” LUS pattern demonstrating the chest wall tissue (subcutaneous tissue and muscles), the pleural line, and below it, echoes that reproduce the pleural line at regular and equal distance intervals echoing the distance between the probe and the pleura. These horizontal artifacts, indicated as A-lines, are visualized when the lung is well aerated.
In a pathological lung when there is loss of aeration and change in the air-fluid balance due to accumulation of subpleural interstitial exudate, transudate, collagen, and blood, for example, the pulmonary surface will no longer behave as a strong reflector of the ultrasound beams. Instead, when the ultrasound beams hit the first area of loss of aeration, there is only partial penetration of the ultrasound energy, creating vertical artifacts on the images which are called b-lines. B-line are defined as discrete laser-like vertical hyperechoic reverberation artifacts that arise from the pleural line, extend to the bottom of the screen without fading, and move synchronously with lung sliding.
Interpretation of LUS in dialytic patients suspicious for COVID‑19
Patients admitted at the dialysis unit and presenting symptoms that raise suspicion of COVID-19 can be first screened with LUS, which can help triaging between low-risk patients and those who show signs of pneumonia and high risk for severe forms of the disease.
Since interstitial pneumonia in COVID-19 is typically peripheral, bilateral, diffuse but asymmetric, it is important to scan initially patients who are admitted to the dialysis unit.
The authors continue to describe in detail the LUS findings of patients with COVID-19 and the workflow of screening patients in the dialysis unit during the pandemic. They conclude that LUS performed by the attending physician represents a safe, inexpensive, easily reproducible technique with a great potential in allowing to differentiate patients with signs of COVID-19 pneumonia.
 English
English
 Español
Español