PERICARDIAL FAT AND CARDIAC FUNCTION • Association of Pericardial Fat with Cardiac Structure, Function, and Mechanics: The Multi-Ethnic Study of Atherosclerosis
Source: J Am Soc Echocardiogr 2022;35:579-87
INTRODUCTION
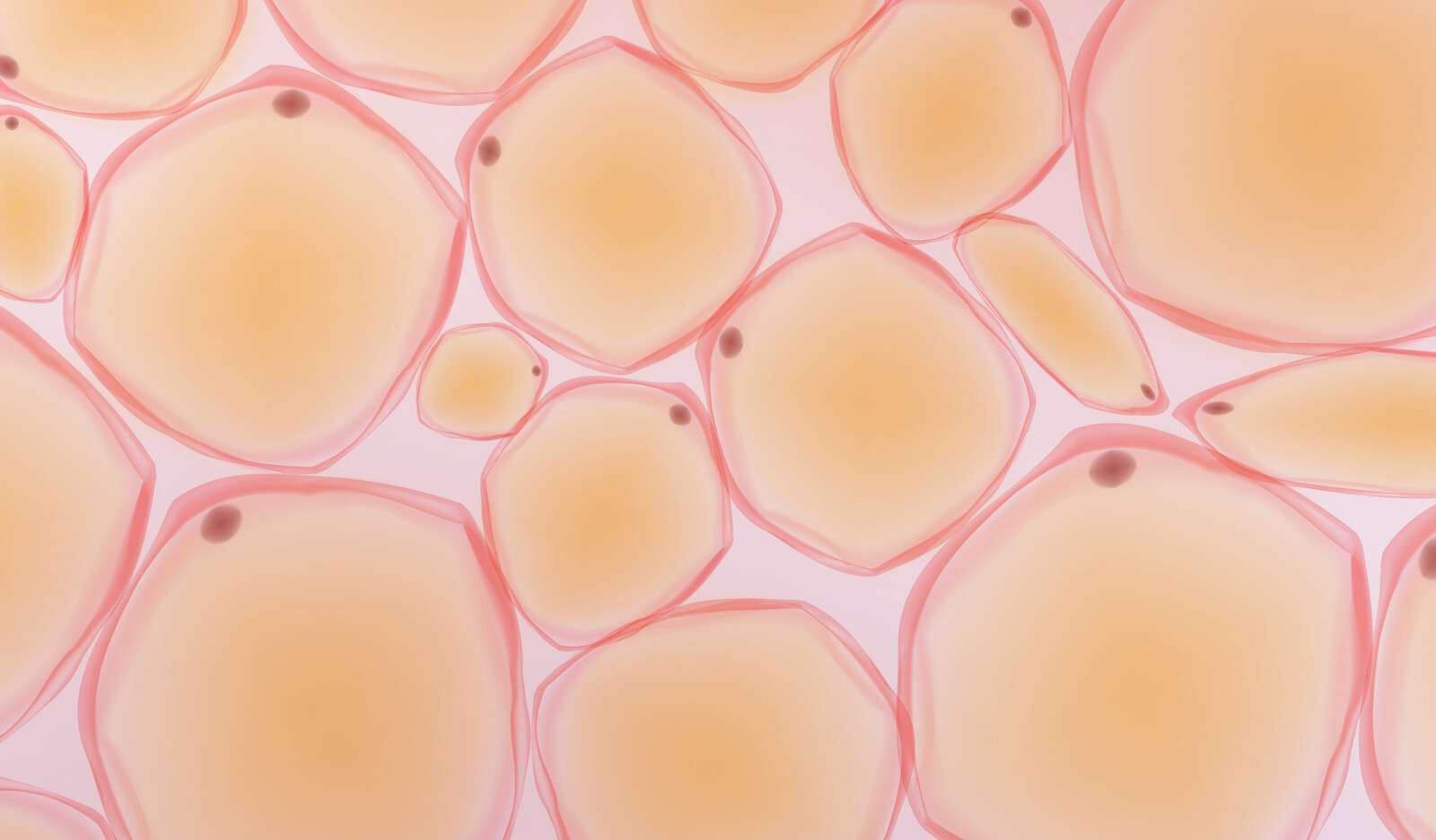
Pericardial adipose tissue – fat superficial to the parietal pericardium (pericardial fat) and fat located between the myocardium and the visceral pericardium (epicardial fat) – has been linked to coronary artery disease, atrial fibrillation (AF), and abnormal cardiac structure and function.
Epicardial fat lies in direct contact with cardiomyocytes and secretes numerous bioactive factors, which have been implicated in adiposity-associated inflammation and insulin resistance. In heart failure with preserved ejection fraction (HfpEF), pericardial adipose tissue is associated with increased cardiac filling pressures and more severe pulmonary hypertension. Excessive adipose tissue around the heart has also been shown to impair ventricular filling by contributing to pericardial restraint in studies of heart failure patients.
Finally, pericardial fat is associated with an increased risk for heart failure in individuals without prior cardiac disease. Therefore, the authors utilized data from the Multi-Ethnic Study of Atherosclerosis (MESA) to examine the association between pericardial adipose tissue volume by computed tomography (CT) with cardiac structure and function by echocardiography.
METHODS
Study Population
MESA is a multicenter prospective cohort study designed to investigate the prevalence, correlates, and progression of subclinical cardiovascular disease in adults without previous clinical cardiovascular disease. comprises 6,814 men and women ages 45-85 years old recruited from six U.S. field sites (Baltimore, Maryland; Chicago, Illinois; Forsyth County, North Carolina; Los Angeles County, California; New York, New York; and St. Paul, Minnesota) and followed over six exams from 2000 to 2018.
Exposure Variable: Pericardial Fat Volume Assessment
Pericardial fat volumes (which include both pericardial and epicardial fat) were determined using volumetric assessment of CT imaging obtained during exam 1 (2000-2002). A subset of participants had repeated assessments at exams 2 (2002-4), 3 (2004-5), and 4 (2005-7).
Outcome Variables
Among MESA participants, 3,032 underwent echocardiography at exam 6 as part of the MESA Early Heart Failure Study, an ancillary study to examine the mechanisms and phenotypes of early heart failure.
RESULTS
3,032 participants who underwent echocardiography at exam 6 were included in the study; 53% female, with mean age 57 years, and 40% White, 25% Black or African American, 22% Hispanic, and 13% Asian.
Baseline (exam 1) pericardial fat volume (mean, 73.6 cm3) was positively correlated with BMI, although there was substantial variation among those with high BMI. Those in the highest quartile of pericardial fat were predominantly male and older, with a greater proportion of White and Hispanic participants, higher BMI, and greater prevalence of baseline cardiovascular risk factors.
Over time, mean pericardial fat volume increased by 1.19 cm3 per year.
In univariate analysis, higher pericardial fat volume at baseline was associated with lower (worse) absolute LV global longitudinal strain and LA reservoir strain, in addition to other indices of LV systolic and diastolic function.
In univariate analysis, increased pericardial fat volume was also associated with lower (worse) absolute RV free wall and right atrial (RA) reservoir strain. Pericardial fat volume was also associated with lower tricuspid annular plane systolic excursion (TAPSE), fractional area change (FAC), and RV s’ velocity. These associations were largely unchanged after further adjusting for pulmonary artery systolic pressure (PASP), LV strain, E/e’ ratio, LA volume, and LA strain.
CONCLUSIONS
The authors concluded that after nearly 20 years of follow-up, in this large, diverse cohort of elderly adults free of baseline cardiovascular disease, pericardial fat volume was associated with distinct atrial and ventricular abnormalities by echocardiography and remained independently associated with cardiac function after adjusting for overall adiposity (i.e., BMI and waist-hip ratio) and other potential confounders.
 English
English
 Español
Español