ORIGINAL INVESTIGATION • Internal Jugular Vein Cannulation Using a 3-Dimensional Ultrasound Probe in Patients Undergoing Cardiac Surgery: Comparison Between Biplane View and Short-Axis View
Source: J Cardiothorac Vasc Anesth. 2021 Jan;35(1):91-97
INTRODUCTION
Compared with the traditional anatomic landmark technique, ultrasound guided IJV cannulation improves patient outcomes by increasing success rates and reducing complications. 2-dimensional (2D) ultrasound-guided techniques include puncturing the IJV in either the short-axis view (SAX) or long-axis (LAX) view. Both techniques have advantages and disadvantages; while the SAX view is easy to perform, tracking the entire needle length is difficult. Though the LAX view may overcome this drawback of the SAX view, the surrounding structures of the vein cannot be seen while the vein is punctured.
The biplane imaging technology in the 3D ultrasound transducer may overcome the spatial limitations of single-plane imaging by providing simultaneous real-time SAX and LAX views on the same screen without altering the transducer position.
The purpose of this study was to compare the efficacy and feasibility of the real-time, 3D ultrasound probe guided BPX view with the universally followed SAX view for IJV cannulation. The primary objectives of the study were to compare the BPX view with the SAX view in terms of time required for imaging, time for IJV puncture, time for guidewire confirmation, number of needle punctures and needle redirections, and incidence of IJV posterior wall puncture. The secondary objectives of the study were to assess the quality of needle visualization during the IJV puncture and the incidence of complications.
METHODS
This was a prospective, observational study of 100 adult patients ages 18-to-70 years, who were scheduled to undergo elective cardiac surgery. The patients were divided into two groups (BPX group and SAX group) of 50 patients each.
In the operating room, general anesthesia was induced, and the patients were positioned in a head down position (20-30 degrees) with the head slightly rotated (30-40 degrees) to the opposite side of cannulation. Aseptic preparation of the neck and chest wall was performed using chlorhexidine solution and sterile drapes.
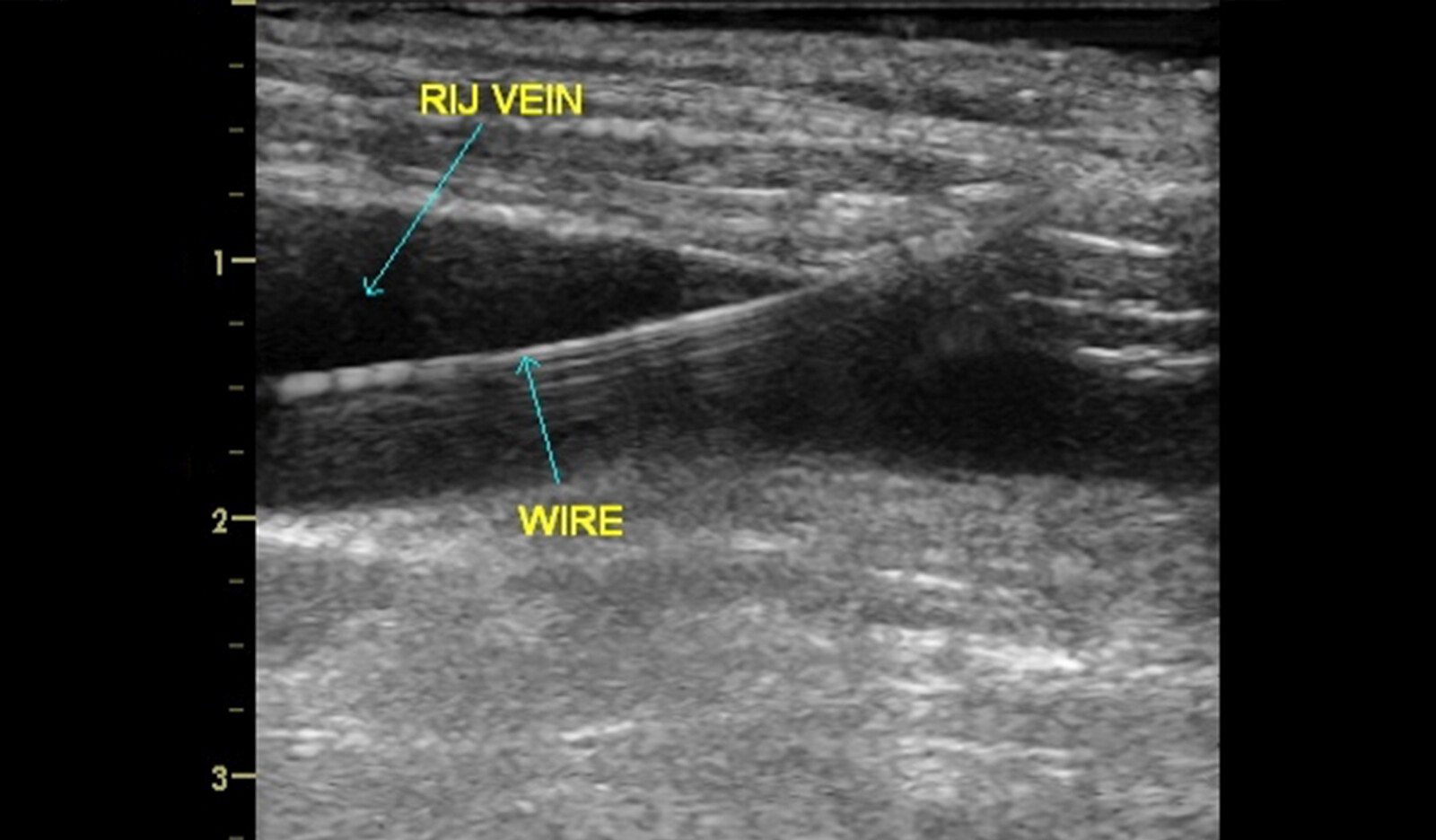
Imaging of the IJV was performed with a 3D phased-array transducer and frequency setting in resolution mode. The ultrasound probe was covered with a sterile plastic sheath before the IJV was imaged. Confirmation of the artery and vein was done by using color and spectral Doppler. Using real-time ultrasound guidance, the IJV was punctured with the needle, and the guidewire was inserted. After confirming guidewire position within the vein using 2D ultrasound, the central venous catheter was placed in the IJV using the Seldinger technique. If the IJV could not be cannulated in 3 attempts, the procedure was abandoned and considered to be a failure, and the opposite side IJV or subclavian vein was cannulated.
Imaging in SAX Group
The SAX image of the IJV was obtained by placing the transducer in transverse alignment on the prepared patient’s neck at the level of the cricoid cartilage. The entry of the needle into the vein was confirmed by visualizing the indentation of the anterior wall of the vein, followed by observing dark colored blood in the syringe and by visualizing the tip of the needle inside the vein.
Imaging in the BPX Group
The BPX imaging of the IJV was obtained by placing the transducer in a transverse alignment on the patient’s neck at the level of the cricoid cartilage. The biplane mode was selected on the ultrasound machine, and the biplane cursor was placed on the SAX view of the IJV. The screen displayed 2 images, with the SAX view of the IJV on left and the LAX view of the IJV on the right. The entry of the needle into the IJV was confirmed by visualizing the indentation of the anterior wall of the IJV in the SAX view and simultaneously visualizing the entire length of the needle entering the IJV in the LAX view.
RESULTS
136 patients were eligible for this study, among whom 36 patients were excluded based on the exclusion criteria. The remaining 100 patients were divided into 2 groups of 50 each. All the IJV cannulations in both groups were right-sided. Diameter of the IJV and margin of safety were similar in both groups.
While the time taken for imaging the IJV was significantly longer in the BPX group than in the SAX group (9.52 ± 2.69 s v 7.94 ± 2.55 s), the time taken for IJV puncture (10.39 ± 2.33 s v 23.7 ± 2.46 s), time taken for confirmation of guidewire (32.94 ± 4.50 s v 57.64 ± 7.14 s), and the incidence of posterior wall puncture (4% v 26%) were significantly less in the BPX group than in the SAX group.
The total number of attempts taken to puncture the IJV was fewer in the BPX group than in the SAX group (55 v 78). Successful puncture of the IJV was done on the first attempt in 90% of patients in the BPX group, whereas it was only 50% in the SAX group.
Quality of needle visualization was good in 90% of patients in the BPX group, whereas only 6% in the SAX group demonstrated good needle visualization. The number of needle redirections for IJV puncture was fewer in the BPX group than in the SAX group (48 v 116).
CONCLUSION
The authors concluded that IJV cannulation with biplane imaging allowed for better clinical performance in terms of less procedure time and fewer cannulation attempts than did SAX imaging in patients undergoing cardiac surgery, without significant difference in the incidence of complications between the 2 groups.
The authors suggested that that biplane imaging can be a safer, feasible and more reliable method for IJV cannulation in cardiac surgical patients.
 English
English
 Español
Español