Original Article: Point-of-Care Ultrasound for the Detection of Hydronephrosis in Emergency Department Patients with Suspected Renal Colic.
Source: Ultrasound J (2020) 12:31
INTRODUCTION
Renal colic is a common presentation in the emergency department (ED), leading to significant utilization of resources, including advanced imaging as well as direct and indirect costs related to patient care and lost work time.
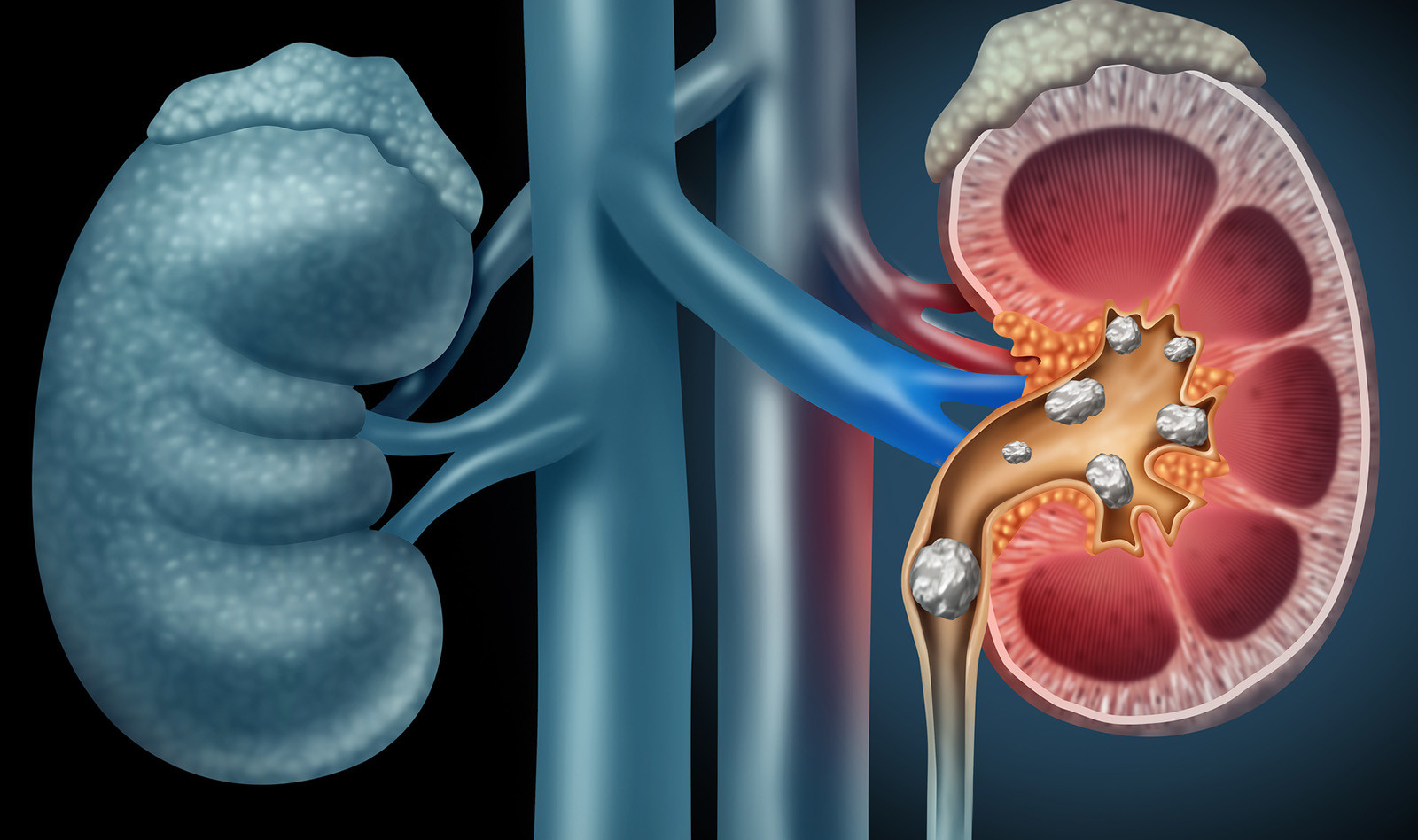
Computed tomography remains the imaging modality of choice to confirm the diagnosis, prognosticate spontaneous stone passage, and rule out other causes of abdominal pain. Alternatively, Radiology ultrasound (radUS) has been proposed as the preferred test for patients at low risk for complications of urolithiasis. Typically, though, the calculus is not seen during the exam and the presence of hydronephrosis is the finding suggesting of ureteric obstruction. Further, point-of-care ultrasound (PoCUS) by emergency physicians has been proposed as an alternative to CT to aid in decision-making in cases of suspected renal colic.
This prospective observational study was performed to determine the diagnostic accuracy of PoCUS for hydronephrosis in patients with suspected renal colic and to evaluated if hydronephrosis diagnosed with PoCUS was predictive of the development of complications.
METHODS
This was a prospective observational study conducted in two academic emergency departments in Ontario. Eligible patients were aged 16–65 years who had either CT or radUS ordered for suspected renal colic. Exclusion criteria included hemodynamic instability, fever, suspected urinary tract infection based on symptoms or urinalysis positive for leukocytes and nitrites, pregnancy, renal transplant, single functioning kidney, known abdominal aortic aneurysm or incarceration.
The PoCUS scans were performed by emergency medicine attendings and residents who had to complete an accredited emergency department ultrasound course or the local, required, introductory point-of-care ultrasound course for emergency medicine residents focusing on focused assessment with sonography in trauma (FAST), aortic and obstetrical ultrasound skills. Scanning physicians had to attend a didactic lecture where the study was described and renal anatomy, ultrasound technique and several examples were reviewed. Newly trained physicians had to complete 25 observed renal ultrasounds with an expert physician (fellowship trained or additional training in renal ultrasound) prior to enrolling patients.
The presence, degree and grading of hydronephrosis was established by a blinded radiologist, who also documented the presence, position and size of any urinary calculus, signs suggestive of recent stone passage, as well as any alternative diagnosis that could account for the patient’s symptoms and the presence of abdominal aortic aneurysm (AAA).
The primary outcome measure was the sensitivity and specificity of PoCUS for the presence or absence of hydronephrosis compared to formal imaging in patients with suspected renal colic. The secondary outcome was the association between PoCUS findings and complications within 30 days, defined as the composite of any urologic intervention (e.g., lithotripsy, stent, or percutaneous nephrostomy), sepsis, hospital admission or death.
RESULTS
Four hundred and fifteen patients were enrolled in the study, out of which 413 patients completed formal imaging and used for the primary analysis of hydronephrosis. Sixty-nine patients lost to follow-up at one month, ending with 344 patients who were used for the secondary analysis.
In total, 17 emergency physicians and residents were eligible to perform renal PoCUS, of which five were considered to be experts.
The sensitivity of PoCUS for the detection of hydronephrosis was 77.1% and the specificity was 71.8%. The sensitivity of PoCUS improved with worsening degrees of hydronephrosis. The presence of hydronephrosis on PoCUS was associated with increased complications (11.8% versus 3.8%), relative risk of 3.1.
CONCLUSION
The authors concluded that PoCUS for hydronephrosis has moderate sensitivity and specificity for renal colic. They believe that these findings limit the utility of PoCUS as a diagnostic test. However, since patients with hydronephrosis are more likely to develop complications, the authors suggest that PoCUS may be useful to help guide further imaging and consultation in combination with clinical course.
 English
English
 Español
Español