Systematic Assessment of the Impact of Ultrasound-Enhancing Agents upon Measurements of Cardiac Size and Function by Echocardiography
Source: J Am Soc Echocardiogr 2020;33:313-21
INTRODUCTION:
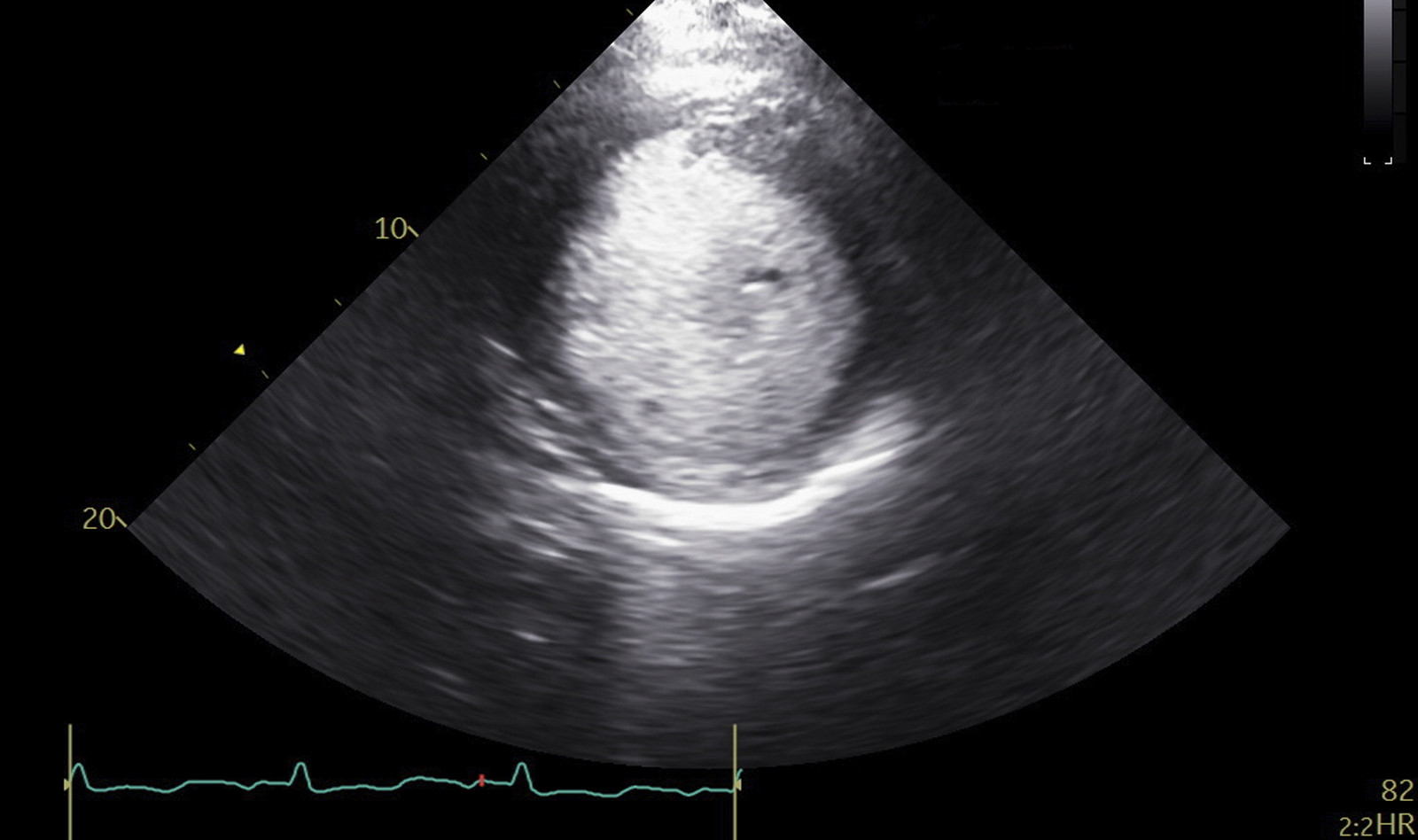
Ultrasound-enhancing contrast agent (CON) is now used routinely to improve both endocardial definition and accurate measurements in patients with suboptimal image quality. Contrast is also useful in the assessment of mass lesions such as apical thrombosis and to distinguish normal structure from artifact and improves the reproducibility of echocardiographic assessment of LV volumes and LV ejection fraction (LVEF).
However, contrast can fill left ventricular intertrabecular recesses, thus yielding larger LV volume compared to two-dimensional (2D) echocardiography. This is practically true in the setting of LV dysfunction and hypertrabeculation.
The purpose of this study was to define the difference between 2D unenhanced echocardiogram and contrast enhanced measures of LV size and function in order to establish reference standards.
STUDY POPULATION
This retrospective study reviewed 3,269 echocardiograms, 624 (21.4%) of which received contrast agent. CON was performed for a variety of indications, including endocardial border definition, enhancement of Doppler signals, identification of cardiac masses (especially apical thrombi) to clarify artifacts, evaluation of apical hypertrophy, and to improve interobserver reproducibility.
2D echocardiography images were adequate from the parasternal long-axis (PLAX) view in 599 cases, 343 of which also had adequate CON images. This allowed for comparison of LV wall thickness and LV dimensions between 2D echocardiography and CON in 343 cases.
In the apical view, images were adequate in 226 cases, 212 of which had adequate CON images, allowing comparison of LV volumes and LVEF between 2D and CON in 212 cases.
RESULTS
Measurements were made only in technically adequate views. The range of LVEF was 10% to 76% (mean, 43 ± 18%), and LVEF < 40% was observed in 231 patients (37.0%). 281 patients in whom the endocardial border could not be defined from either apical two-or four-chamber views were excluded from the study.
Cardiac dimensions and wall thickness were measured and analyzed in 343 cases in the PLAX view. Clear endocardial borders were observed in 212 patients for both 2D echocardiography and CON in the apical view, and these were analyzed for LV volumes and LVEF. The following highlights the major result of this study:
- The correlation between 2D echocardiography and contrast echocardiography was greater for LV dimensions and volumes than for LV wall thickness.
- Wall thickness values of the interventricular septum and posterior wall by 2D echocardiography were greater than those by contrast echocardiography.
- Left ventricular end-diastolic dimensions (LVEDD) and left ventricular end-systolic dimensions (LVESD) by 2D echocardiography were less than those by contrast echocardiography.
- Left ventricular end-diastolic volumes (LVEDV) and left ventricular end-systolic volume (LVESV) by 2D echocardiography were less than those by contrast echocardiography.
- Left ventricular ejection fraction (LVEF) was higher by 2D echocardiography than by contrast echocardiography.
The authors pointed out that previously published papers on this topic had smaller study population, were limited in scope and used fewer views. In contrast to previous studies, this study included also the parasternal views, which are important for wall thickness measurements, especially when the apical window is not available.
In addition, this study analyzed the relationship of contrast and 2D echocardiography to BMI and sex and found that patients with BMI > 30 kg/m2 had a larger difference in LVEF between contrast and 2D echocardiography than those with BMI < 25 kg/ m2. Finally, this study also found that 7% of patients with LVEF > 50% measured in 2D echocardiography had LVEF < 50% with contrast. While this difference is small, it could yield an erroneous echocardiographic diagnosis that could affect clinical management.
 English
English
 Español
Español