THE HEMODYNAMIC CORNER • Aortic Stenosis Severity: Rhythm Makes a Difference
Source: CASE: Cardiovascular Imaging Case Reports. 2022;6(8):382-366
INTRODUCTION
The assessment of aortic valve stenosis (AS) severity based on Doppler velocity and pressure gradient is flow dependent. Both velocity and pressure gradient increase with elevated transaortic flows and decrease with reduction in flow rates for a given aortic valve orifice area.
Therefore, during high-flow states the assessment of the true severity of AS should be carefully performed.
In this case report, the authors describe a challenging case of assessing AS severity in the setting of bradycardia from complete heart block (CHB), normal left ventricle (LV) function, permanent atrial fibrillation (AF), and moderate AS at baseline.
Case presentation
History of Present Illness
During the initial evaluation of a 74-year-old male who was admitted for evaluation of recurrent falls he was found to be in complete heart block with ventricular rate of 35-40 bpm. His past medical history was significant for atrial fibrillation, CABG (6 months prior to admission), stage 3 chronic kidney disease, diabetes mellitus, hypertension, and hyperlipidemia.
Investigations and Clinical Course
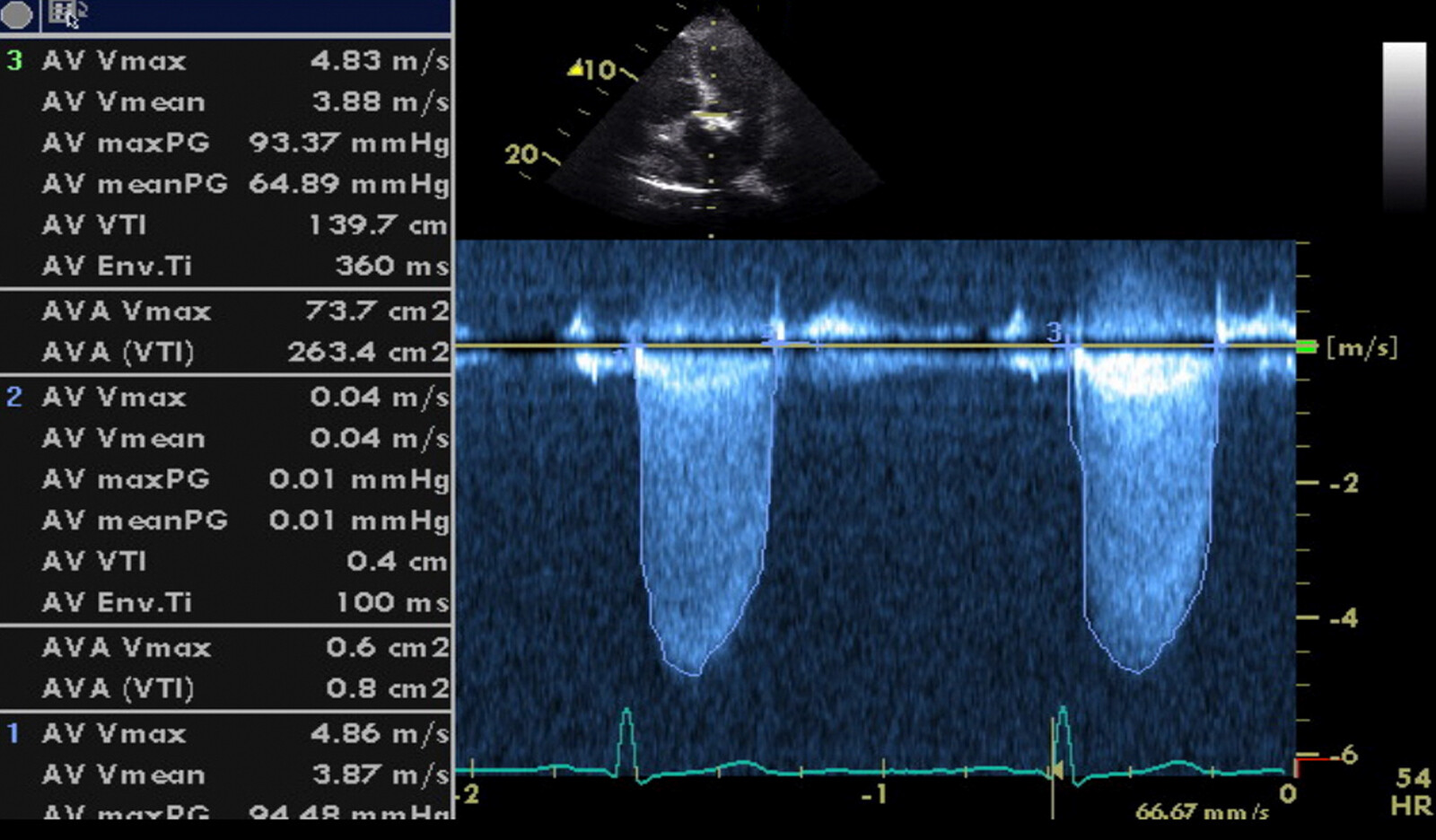
Initial transthoracic echocardiogram (TTE) demonstrated normal left ventricular (LV) systolic function, dilated left atrium, LV outflow track (LVOT) diameter of 2.2 cm, and a calcified restricted aortic valve.
Severe AS was considered based on transaortic valve indices (peak velocity [PV] = 4.8 m/sec and mean pressure gradient = 48 mm Hg), LVOT velocity time integral (VTI) was 32 cm, and aortic valve VTI was 116 cm with a stroke volume of 124 mL. The calculated aortic valve area by continuity equation was 1.06 cm 2 with a dimensionless valve index (DVI) of 0.27.
The management of complete heart block was with placement of a permanent pacemaker. It was also recommended to have a workup for transcatheter aortic valve implantation.
Right heart catheterization revealed patent coronary artery grafts and normal filling pressures (right atrial = 4 mm Hg, right ventricle = 30/4 mm Hg, pulmonary artery = 29/10 mm Hg, pulmonary capillary wedge pressure = 10 mm Hg), and estimated cardiac output was 5.9 L/min at an average heart rate of 79 bpm.
Mean aortic valve gradient was 21 mmHg, and valve area was 1.4 cm2 on invasive assessment consistent with moderate AS. Left ventricular end-diastolic pressure was 7 mm Hg.
Findings on repeated TTE were very similar to aortic valve parameters measured during cardiac catheterization (PV = 3.4 m/sec, mean pressure gradient = 25 mm Hg) and moderate-grade AS. The LVOT VTI, aortic valve VTI, and stroke volume decreased to 18 cm, 64 cm, and 71 ml, respectively. Consequently, the aortic valve area and DVI increased to 1.1 cm2 and 0.29, respectively.
Both cardiac catheterization and new TTE exam confirmed improvement in AVA and the degree of stenosis was changed from severe to moderate after pacemaker placement.
The initial plans for transcatheter aortic valve replacement were postponed.
DISCUSSION
The authors then discuss the limitations of Doppler assessment of AVA in some cases, such as this one. While there are many parameters that are measured during TTE evaluation of AS, peak velocity and mean pressure gradient are the most widely used. Since measurements are dependent on flow rate across the aortic valve, in certain unique scenarios (such as in this case), these values may be falsely elevated.
This patient with pre-existing moderate aortic stenosis, preserved LV systolic function and permanent AF, presented with complete heart block and severe bradycardia. The end result was increased diastolic filling, which in turn led to an elevated stroke volume, increased flow across the aortic valve and over estimation of severity of aortic stenosis.
CONCLUSION
The authors emphasized the importance of understanding the role of increased blood flow across the aortic valve that may be seen in complete heart block, and how this may lead to over estimation of severity of aortic stenosis.
 English
English
 Español
Español