CASE STUDY • ‘Hydro-point’ – The Forgotten and Unspoken Entity in Hydropneumothorax
Source: AJUM November 2021;24(4);246-248
CASE REPORT
A 30-year-old chronic smoker presented to the emergency department with a history of breathlessness, cough with expectoration, and right-sided chest pain for the past four days. On initial assessment, the patient’s saturation was low (50% in room air), and right-sided air entry was absent.
After starting the patient on high flow oxygen saturation improved to 90%. Other assessments and vital signs were normal.
Lung point-of-care ultrasound (POCUS) showed hydro-point, dynamic air–fluid interface (DAFI) sign and a characteristic triple sign, namely barcode sign/stratosphere sign, hydro-point and sinusoidal pattern in right lung. These features are seen in effusive pneumothorax, namely hydropneumothorax, hemopneumothorax and pyopneumothorax.
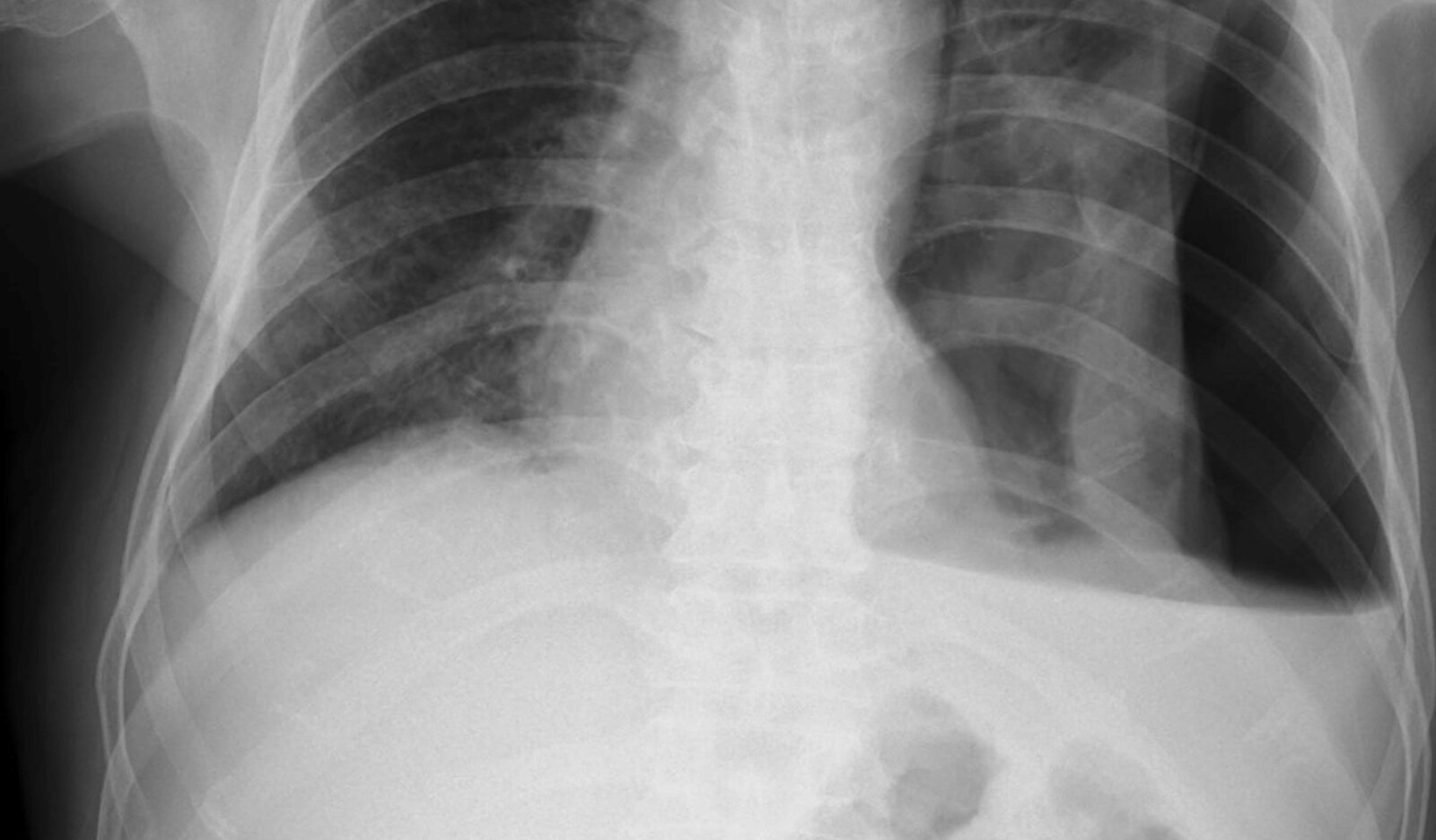
Chest X-ray findings – Chest X-ray showed air–fluid level, which confirmed effusive pneumothorax as predicted by POCUS.
A right-sided intercostal tube drainage (ICD) was inserted, which had a gush of air and straw-colored fluid confirming it as hydropneumothorax, followed by a CXR to check for tube position. The patient’s saturation improved to 96% and was symptomatically better after ICD. Baseline workup showed raised white blood cell counts. Sputum acid-fast bacilli staining (AFB) was positive for mycobacterium tuberculosis. The patient’s pleural fluid culture–sputum culture turned out to be positive for pseudomonas aeruginosa and klebsiella pneumoniae co-infection and he was started on appropriate antibiotic therapy. The final diagnosis was tubercular hydropneumothorax with secondary bacterial infections.
DISCUSSION
The authors discuss the simultaneous demonstration on lung ultrasound signs of pneumothorax in the nondependent zone and pleural effusion signs in the dependent zone and suggest that this pattern may hint towards hydropneumothorax.
They describe the ultrasound technique for confirming hydropneumothorax at the bedside, by slowly screening the lung with ultrasound in the caudocranial direction in sitting position from the effusion zone.
At the air–fluid interface level one can see hyperechoic anechoic dynamic image subpleurally, which is called hydro-point and DAFI sign. Thus, if such a pattern of barcode sign or absent lung sliding in the non-dependent zone, hydro-point at interface zone and pleural effusion/sinusoidal pattern in the dependent zone are seen, hydropneumothorax can be diagnosed at the bedside.
The authors also commented that ultrasound in peripherally located larger lung abscess may also show hydro-point, which requires further ultrasonographic research studies.
Finally, they discuss the potential benefit of using these signs when scanning patients with lung ultrasound in India, since the most common cause of hydropneumothorax in India is tuberculosis. Other causes of hydropneumothorax are necrotizing bacterial pneumonia, obstructive lung disease, bronchopleural fistula, esophago-pleural fistula, prior lung surgery, lung malignancy, iatrogenic causes, chest trauma, cystic lung disease, pulmonary infarction, post-partial pneumonectomy and rarely connective tissue disorders.
 Español
Español
 English
English