CLINICAL INVESTIGATIONS • Passive Leg Raise Stress Echocardiography in Severe Paradoxical Low-Flow, Low-Gradient Aortic Stenosis
Source: J Am Soc Echocardiogr 2022;35:1123-32
INTRODUCTION
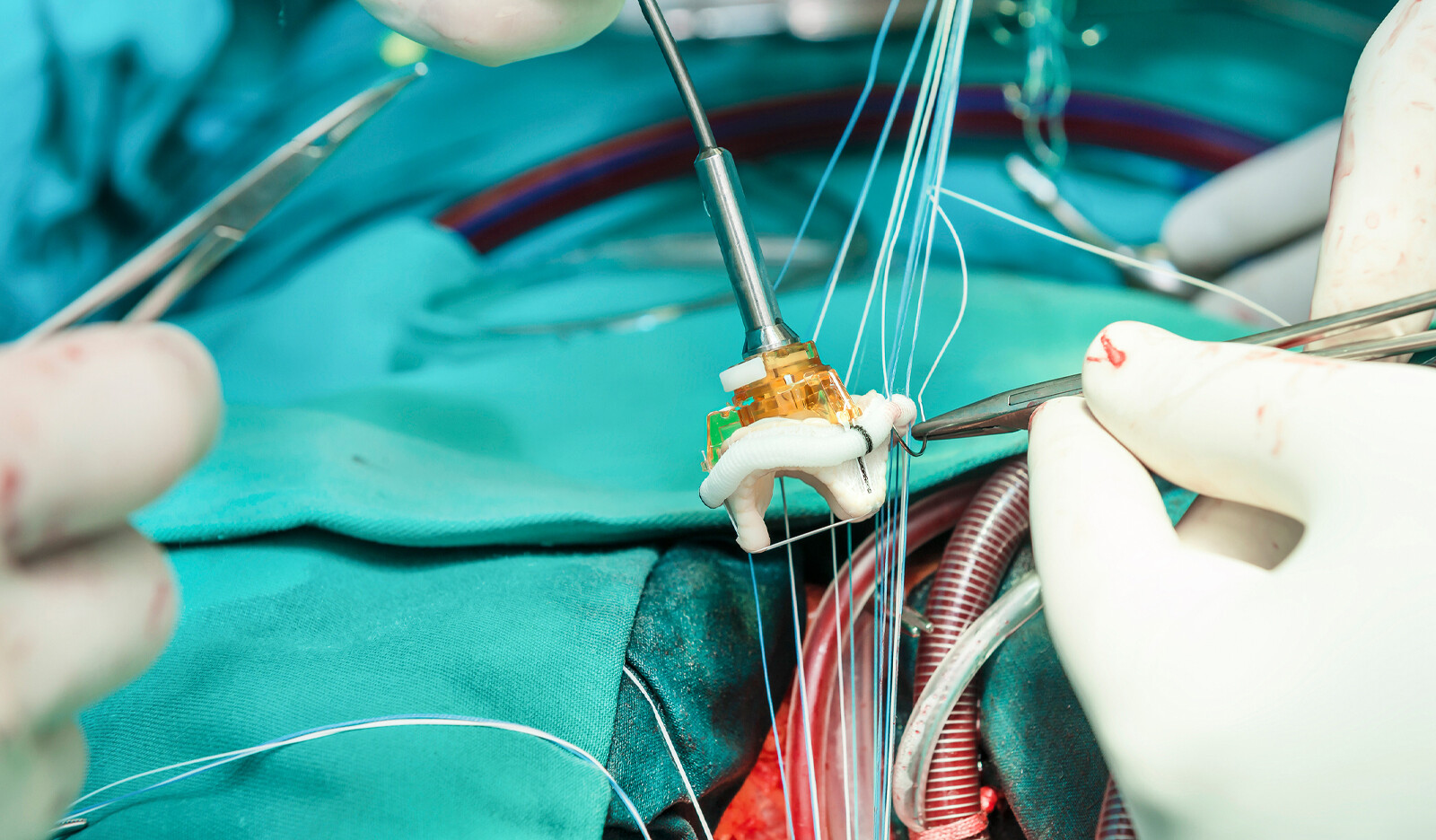
Management of aortic stenosis (AS) – the most common valvular heart disease in Europe and North America – is done by catheter intervention or surgery; in severe symptomatic AS, valve replacement is the treatment of choice. Diagnosis of severe AS, which is defined as an aortic valve area (AVA) ≤ 1.0 cm2, is done with echocardiography.
The left ventricle (LV) ability to produce transvalvular flow that is sufficient in generating high gradients varies. Therefore, AVA calculations with echocardiography does not closely correlate with transvalvular pressure gradients.
To account for this, subcategories of severe AS have been introduced and include:
- “Classical” low-flow, low-gradient AS, in which left ventricular ejection fraction (LVEF) is reduced (stroke volume index (SVI) ≤ 35 mL/ m2 body surface area)
- ‘‘Paradoxical’’ variant, where the LVEF is normal (mean transvalvular pressure gradient < 40 mm Hg)
In some of these patients, calculated valve area increases if the low transvalvular flow can be increased. Dobutamine stress echocardiography has therefore been proposed to unmask preserved cusp mobility by provoking a sufficient increase of SVI resulting in an AVA of >1 cm2.
It has been shown, though, that the use of Dobutamine does not increase SVI significantly in up to one third of patients undergoing low-dose dobutamine stress echocardiography. Dobutamine induces ventricular unloading by its ß2-sympathomimetic action with venous vasodilation, manifesting as decreased pulmonary capillary wedge pressure but also as more prevalent dynamic intraventricular obstruction.
For these reasons, dobutamine stress echocardiography is not typically used in patient with paradoxical low-flow, low-gradient AS. A volume challenge, on the other hand, is expected to counteract these mechanisms and could therefore be helpful in those patients.
The aim of this study was to test the passive leg raise (PLR) – a reversible volume challenge – in addition to dobutamine for its ability to increase SVI and transvalvular flow in patients with severe paradoxical low-flow, low-gradient AS.
METHODS
Study Design and Patient Selection
This observational cohort study was conducted prospectively in 45 consecutive patients with severe low-flow, low-gradient AS, defined as a combination of AVA 1 ≤ cm2, mean transvalvular gradient < 40 mm Hg on continuous-wave Doppler echocardiography, and SVI ≤ 35 mL/m2.
Exclusion criteria included:
- LVEF <20%
- Known severe three-vessel coronary artery disease
- More than mild aortic regurgitation
- More than mild mitral valve disease
- Unstable angina pectoris
- Acute pulmonary edema
- Signs of congestive heart failure
- Severe pulmonary, renal, or hepatic disease
Stress Echocardiographic Protocol
The stress echocardiographic examinations consisted of a four-step procedure:
- Rest: Measurements were taken at rest with the patient in a horizontal supine position
- PLR: The patient’s legs were passively lifted by approximately 70°, and the upper body was reclined approximately 20° in a Trendelenburg position
- Maximal dobutamine infusion rate (Dmax): After restoring the horizontal resting position and waiting for volume redistribution (5 minutes), intravenous dobutamine infusion was started at 10 mg/kg/ min and increased by 5 mg/kg/min every 5 minutes up to a maximal target dose of 20 mg/kg/min
- Dmax+PLR: The unaltered dobutamine infusion rate then was combined with the postural changes described in step 2
Analysis of Echocardiographic Images
The following parameters were retrieved and analyzed using TomTec Arena software:
- Pulsed-wave Doppler velocity-time integral (VTI) of flow in the LVOT (VTILVOT) and the corresponding ejection time
- LVOT diameter (inner edge to inner edge, in mid-systole, within 0.5-1 cm of the valve orifice)
- Continuous-wave Doppler VTI as well as the gradients across the AV (VTIAV)
- LV end-diastolic volume (LVEDV) and LVend-systolic volume using the Simpson method
Two methods for calculating SV were used:
- VTI method: SV = VTILVOT x (LVOT diameter/2)2
- Simpson method: SV = LVEDV – LV end-systolic volume
Study End Points
The primary end point was the change in SVI during the stress maneuvers (steps 2-4) compared with resting conditions (step 1).
The secondary study end points were:
- The change in transvalvular flow during the stress maneuvers compared with resting conditions
- The difference between Dmax and Dmax+PLR (steps 3 and 4)
Two common methods for calculating both study end points were used: the VTI and the Simpson methods.
RESULTS
Out of the 45 patients were ultimately recruited for the study, 25 were categorized as belonging to the paradox group and 20 to the low EF group.
The individual Dmax was 20, 15, and 10 mg/kg/min in 19, one, and five patients in the paradox group and in 15, two, and three patients in the low EF group, respectively.
The reasons for not further increasing dobutamine rate were:
- Occurrence of supraventricular or ventricular premature contractions or tachycardia (n = 6)
- High blood pressure (n = 1)
- Low blood pressure (n = 2)
- Reaching maximal heart rate (n = 2)
There were no significant differences between the groups with respect to demographics, cardiovascular risk factors, and medications, except for a larger proportion in the low EF group taking P2Y 12 inhibitors and angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers.
The two groups differed in the echocardiographic parameters specific for group assignment, such as LVEF and LV volumes. Although no patient had an SVI VTI above 35 mL/m2 by definition, it was significantly lower in the low EF group at rest than in the paradox group.
The mean AV pressure gradient and the SVI measured invasively substantially differed between paradox group and low EF group (mean gradient, 27 ± 13 vs 18 ±10 mm Hg [P = .025]; mean SVI, 30 ± 3 vs 27 ± 5 mL/m2[P < .001]).
AVA according to the Gorlin formula did not significantly differ between the paradox and low EF groups (0.87 ± 0.34 vs 0.94 ± 0.46 cm2, P = .65).
Paradox Group
There was a significant decrease in LVEDV compared with rest under Dmax (61 ± 15 vs 49 ± 18 mL, P < .001), which was fully restored with Dmax+PLR (61 ± 15 vs 61 ± 18 mL, P = 1.00) in the paradox group.
The only stress maneuver that resulted in a significant increase in LVEDV compared with rest was PLR (61 ± 15 vs 72 ± 17 mL, P < .001).
LVEDV significantly increased from Dmax to Dmax+PLR (49 ± 18 vs 61 ± 18 mL, P < .001). PLR alone had also a significant effect in increasing SVI compared with rest, irrespective of the measurement method (VTI, 32 ± 3 vs 38 ± 4 mL/m2[P < .001]; Simpson, 24 ± 5 vs 28 ± 6 mL/m2[P < .001]).
With Dmax, no statistically significant change in SVI could be observed for the Simpson method, but an increase was observed for the VTI method (32 ± 3 vs 36 ± 7 mL/ m2, P = .02). Among all stress maneuvers, SVI was lowest during Dmax for both measurement methods.
CONCLUSIONS
The authors concluded that volume challenge such as PLR combined with low-dose dobutamine during stress echocardiography enhances the hemodynamic stimulus desired for detecting severe low-flow, low-gradient AS.
Further, this hemodynamic effect is particularly pronounced in the paradoxical form of stenosis because PLR fully compensates for the unwanted reduction in preload caused by dobutamine, as demonstrated by the marked reduction of LVEDV under dobutamine alone and its restoration when combined with PLR.
In summary: Dobutamine decreases preload in paradoxical low-flow, low-gradient AS, but adding PLR restores the original LV volume, thereby supporting the desired stimulus in terms of SVI and flow increase.
Therefore, this additional stress maneuver should be considered in these patients and is more likely to categorize the majority of those patients as belonging to the pseudosevere group.
 Español
Español
 English
English