Incidence of Stress Cardiomyopathy During the Coronavirus Disease 2019 Pandemic
Source: JAMA Network Open. 2020;3(7):e2014780.
INTRODUCTION
The effect of COVID-19 pandemic has significant social, economic, and cultural ramifications beyond healthcare challenges, and has been linked with increasing stress and anxiety worldwide. Recent reports suggest that the incidence of stress cardiomyopathy (also known as Takotsubo cardiomyopathy) may have gone up during the COVID-19 crisis. The mechanism associated with COVID-19 causing stress cardiomyopathy may be related to psychological, social, and economic stress with imposed quarantine, lack of social interaction, strict physical distancing rules, and its economic consequences in people’s lives.
This study investigated the incidence of stress cardiomyopathy during the COVID-19 pandemic and compared it to historical cohorts.
STUDY POPULATION
This was a retrospective analysis of electronic medical records. The study group was of all patients presenting with acute coronary syndrome (ACS) during the COVID-19 pandemic between the dates of March 1 to April 30, 2020. The control group was of patients presented with ACS in March and April of 2018, 2019 and 2020.
DIAGNOSTIC CRITERIA
The diagnosis of stress cardiomyopathy was based on the international Takotsubo syndrome diagnostic criteria from 2014 (European Heart Journal (2018) 39, 2032–2046), and included:
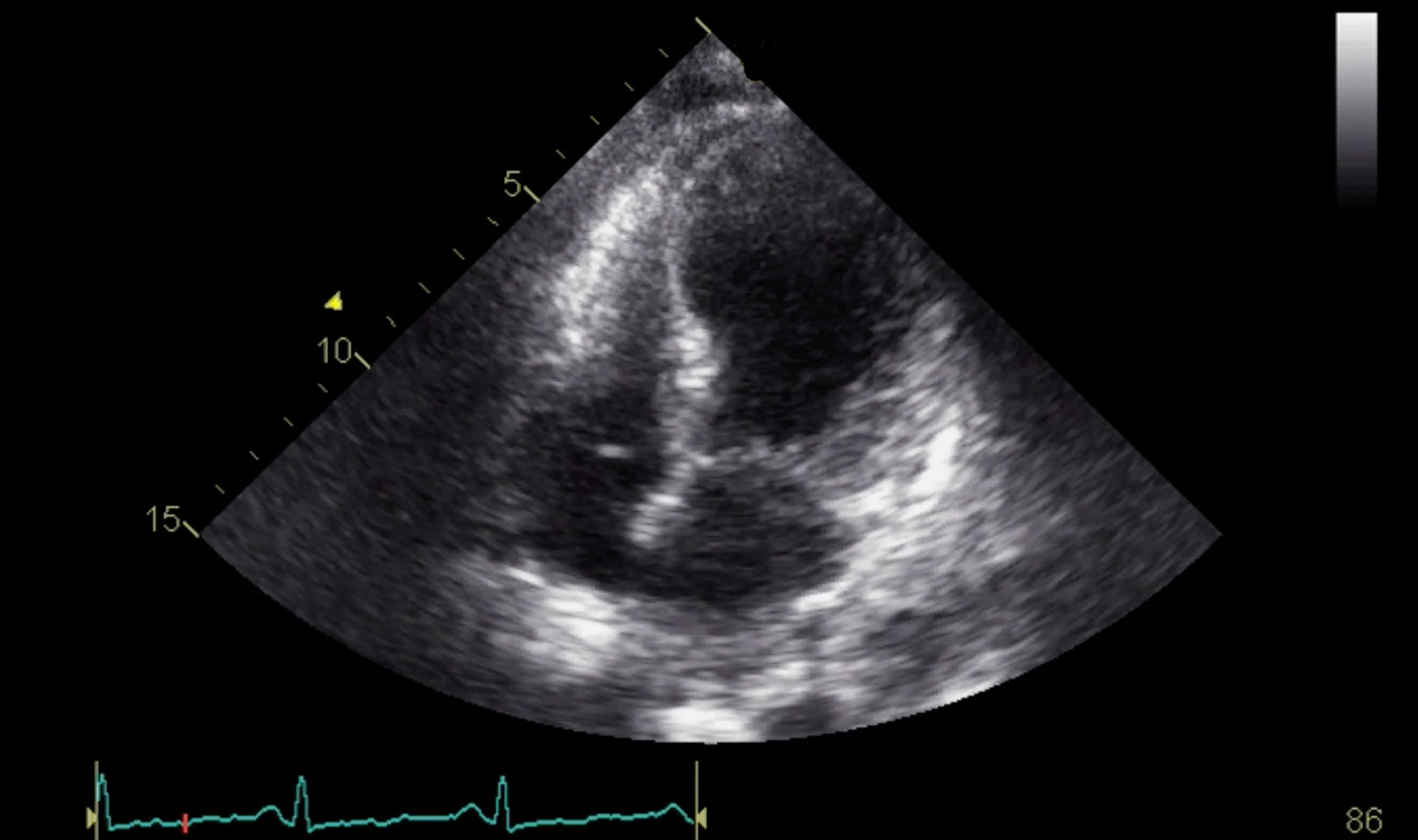
- Transient left ventricular dysfunction (hypokinesia, akinesia, or dyskinesia) presenting as apical ballooning or midventricular, basal, or focal wall motion abnormalities. Right ventricular involvement can be present.
- An emotional, physical, or combined trigger can precede the takotsubo syndrome event, but this is not obligatory.
- Neurologic disorders (e.g. subarachnoid hemorrhage, stroke/transient ischemic attack, or seizures) as well as pheochromocytoma may serve as triggers for takotsubo syndrome.
- New ECG abnormalities are present (ST-segment elevation, ST-segment depression, T-wave inversion, and QTc prolongation); however, rare cases exist without any ECG changes.
- Levels of cardiac biomarkers (troponin and creatine kinase) are moderately elevated in most cases; significant elevation of brain natriuretic peptide is common.
- Significant coronary artery disease is not a contradiction in takotsubo syndrome.
- Patients have no evidence of infectious myocarditis.
- Postmenopausal women are predominantly affected.
RESULTS
1914 patients who were admitted with ACS were included in the final analysis. The control group included 1656 patients who were admitted during the pre–COVID-19 period. The study group included 258 patients who were admitted during the COVID-19 period. The two groups were appropriately matched.
Patients in the study group (patients presenting with ACS during the COVID-19 period) had significant increase in the incidence of stress cardiomyopathy. A total of 20 patients (incidence proportion, 7.8%) in the study group had stress cardiomyopathy, compared with 5 to 12 patients (incidence proportion range, 1.5%-1.8%) in the control group (pre-COVID-19 period).
Other findings included lower median initial troponin and peak troponin levels for patients in the study group compared with the control group and longer median hospital length of stay for patients in the study group compared with those hospitalized in the pre-pandemic period.
There were no significant mortality differences or 30-day rehospitalization rate between the study and control groups.
CONCLUSIONS
The authors believe that this is the first study that systematically investigated the association of the incidence of stress cardiomyopathy with the psychological, social, and economic stress associated with the COVID-19 pandemic.
This study provides an insight into the increasing incidence of stress cardiomyopathy during the COVID-19 pandemic, where the incidence of stress cardiomyopathy was significantly higher in patients presenting with ACS during the pandemic, when compared to the control group during the pre-pandemic period.
The authors conclude that given the negative COVID-19 testing results in all patients diagnosed with stress cardiomyopathy in the study group, the psychological, social, and economic distress accompanying the pandemic, rather than direct viral involvement and sequelae of the infection, are more likely factors associated with the increase in stress cardiomyopathy cases
 Español
Español
 English
English