Right Ventricular Postsystolic Strain Curve Morphology before and after Vasodilator Treatment in Idiopathic Pulmonary Arterial Hypertension
Source: CASE: Cardiovascular Imaging Case Reports Volume 6 Number 5:228-232
INTRODUCTION
A 37-year-old woman presented at the cardiology outpatient clinic for exertional dyspnea (World Health Organization functional class III) and effort syncope 2 months after giving birth. Physical examination revealed no peripheral edema, murmur, or pulmonary crackles. She was well perfused, and oxygen saturation was 99% on room air. An electrocardiogram showed negative T waves in right precordial and inferior leads.
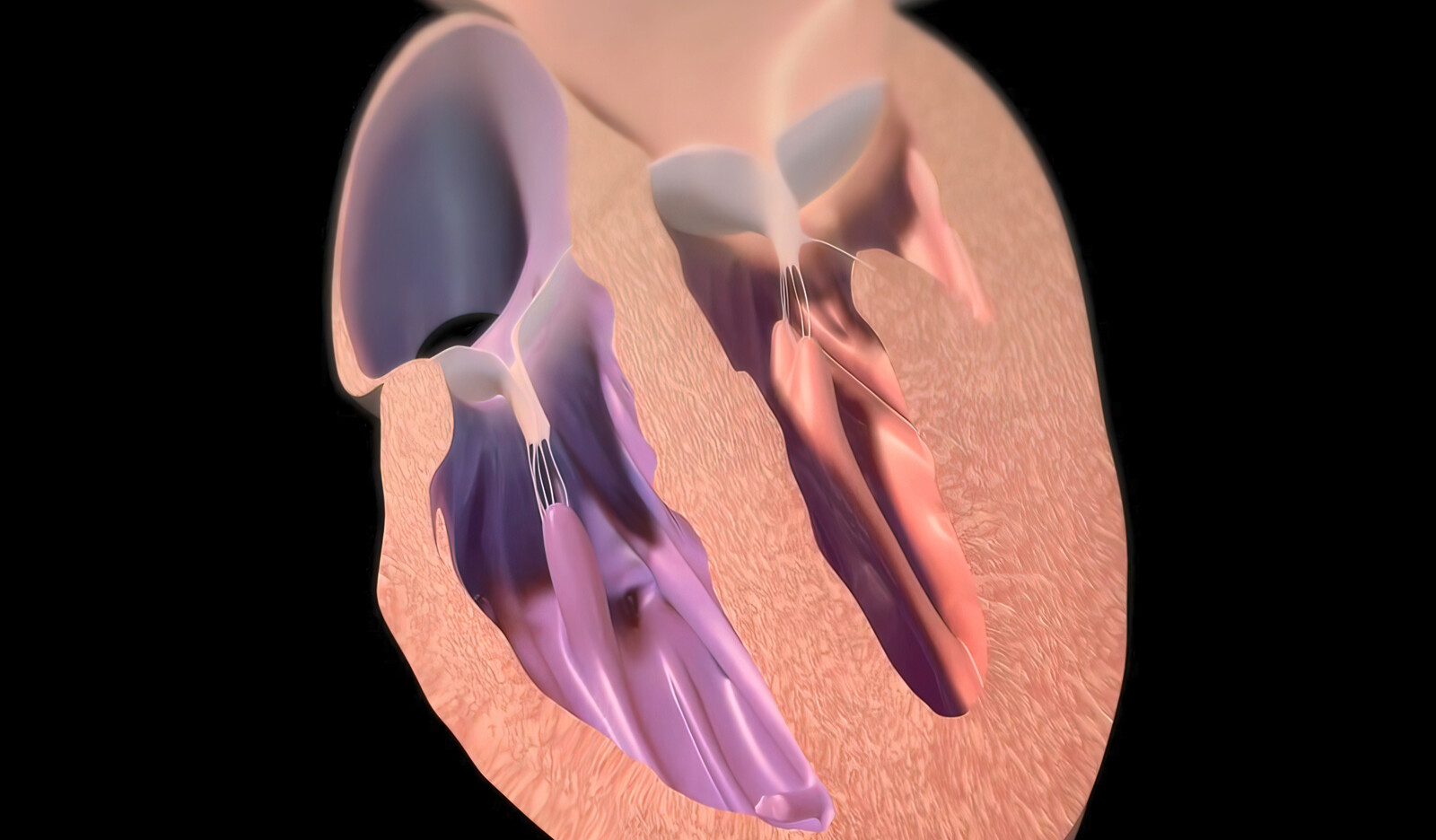
An echocardiogram showed RV dilatation with RV end-diastolic area of 30.1 cm2, RV midcavity diameter of 43 mm, and basal diameter of 42 mm. It also showed mild RV dysfunction with FAC of 31%, TAPSE of 21 mm, and TDI S’ of 13 mm/sec, a prominent systolic D shape suggesting pressure overload, moderate tricuspid regurgitation, and estimated pulmonary artery (PA) systolic pressure (PASP) of 73 mm Hg with a nondilated and collapsible inferior vena cava of 1.6 cm.
Investigations
The authors thought that the main differential diagnosis was pulmonary embolism, but a computed tomography angiography showed no evidence of pulmonary embolism, but the main PA was dilated (38 mm). There was no parenchymal lung disease, anomalous pulmonary venous drainage, or interatrial or interventricular communication.
Right heart catheterization showed severe precapillary pulmonary hypertension (PASP, 98 mm Hg; diastolic PA pressure, 43 mm Hg; mean PA pressure, 66 mm Hg; wedge pressure, 10 mm Hg; cardiac output, 5.3 L/minute; cardiac index, 3.25 L/minute/m2, and pulmonary vascular resistance, 11 Wood units).
Idiopathic pulmonary arterial hypertension was diagnosed based extensive workup.
The RV functional assessment was completed with a strain analysis showing an RV free-wall longitudinal strain (RVFWLS) of –19.4% (normal value, –37.2% to –20.8% from the World Alliance of Societies of Echocardiography study and a type II postsystolic strain pattern
Management
The patient started daily treatment with ambrisentan 10 mg and tadalafil 40 mg. Six months later, her symptoms had improved to World Health Organization functional class I and NT-proBNP was normal (118 ng/L).
A follow-up serial echocardiogram showed the RV was less dilated (RV end-diastolic area, 21.1 cm2; RV midcavity diameter, 35 mm; basal diameter, 41 mm) with preserved systolic function (FAC, 40%; TAPSE, 24 mm; and TDI S’, 15 mm/sec.
Tricuspid regurgitation was mild, inferior vena cava measured 1.5 cm and inspiratory collapse was present, and PASP was estimated at 73 mm Hg just as previously seen. Right ventricular strain improved, showing an RVFWLS of –27% and a type I postsystolic strain pattern. The TAPSE/PASP ratio showed an improvement from 0.28 to 0.33. Left ventricle parameters remained unaffected (end-diastolic biplanar volume of 58 mL and LV ejection fraction of 63%).
DISCUSSION
The authors discussed the current guidelines for diagnostic workup of pulmonary hypertension, which include right heart catheterization to establish diagnosis, a transthoracic echocardiography to rule out left heart disease, a ventilation/perfusion lung scan to exclude chronic thromboembolic pulmonary hypertension, a chest computed tomography scan and pulmonary functional tests to exclude parenchymal lung disease, and routine screening of connective tissue disease, hepatitis, and HIV.
They also describe a recent report describing the prognostic impact of three postsystolic strain patterns of the RV free wall in a cohort of patients with IPAH reflecting progressive RV dyssynchrony.
Pattern I was defined as a strain-time curve with a prompt downward return to baseline after the systolic peak with an end-diastolic straight line. This finding was associated with normal RV size and function. Pattern II corresponded to a strain-time curve with a postsystolic plateau followed by a return to baseline in end diastole. Pattern III was defined as a postsystolic curve slowly and gradually moving toward baseline. This pattern was associated with severe functional class deterioration and severe RV dilation and dysfunction. It predicted worse clinical outcomes than pattern II.
In this study, the authors report a case of IPAH with RV dilation and mild RV dysfunction parameters with mildly reduced FAC and RVFWLS but normal TAPSE and TDI S’; in addition to these findings, the postsystolic strain pattern type II suggested a poor prognosis. Pulmonary vasodilator treatment was initiated with good clinical response, and the RV strain postsystolic pattern changed from pattern II to pattern I within 6 months.
Remarkably, RV echocardiographic improvement paralleled functional class improvement, despite the lack of a significant reduction in the estimated PASP. In addition, there was a mildly improved TAPSE/PASP ratio, which suggested an improvement in the RV-PA coupling.
CONCLUSION
The authors concluded that no single echocardiographic parameter is sufficiently accurate to evaluate RV function, and an integrative approach is usually needed.
They also believe that right ventricular postsystolic strain patterns add a new tool to assess RV compromise in IPAH and may be of interest in addition to other parameters to identify RV dysfunction early, establish prognosis, and guide patient response to treatment.
 Español
Español
 English
English