CLINICAL INVESTIGATIONS • Comparison of Mitral Regurgitant Volume Assessment between Proximal Flow Convergence and Volumetric Methods in Patients with Significant Primary Mitral Regurgitation: An Echocardiographic and Cardiac Magnetic Resonance Imaging Study
Source: J Am Soc Echocardiogr 2022;35:671-81
INTRODUCTION
Assessment of primary mitral regurgitation (MR) severity is of paramount importance for clinical decision-making to determine the optimal timing of surgical intervention in these patients. Current guidelines recommend determination of mitral regurgitant volume (RVol) as part of the thorough assessment of the severity of MR.
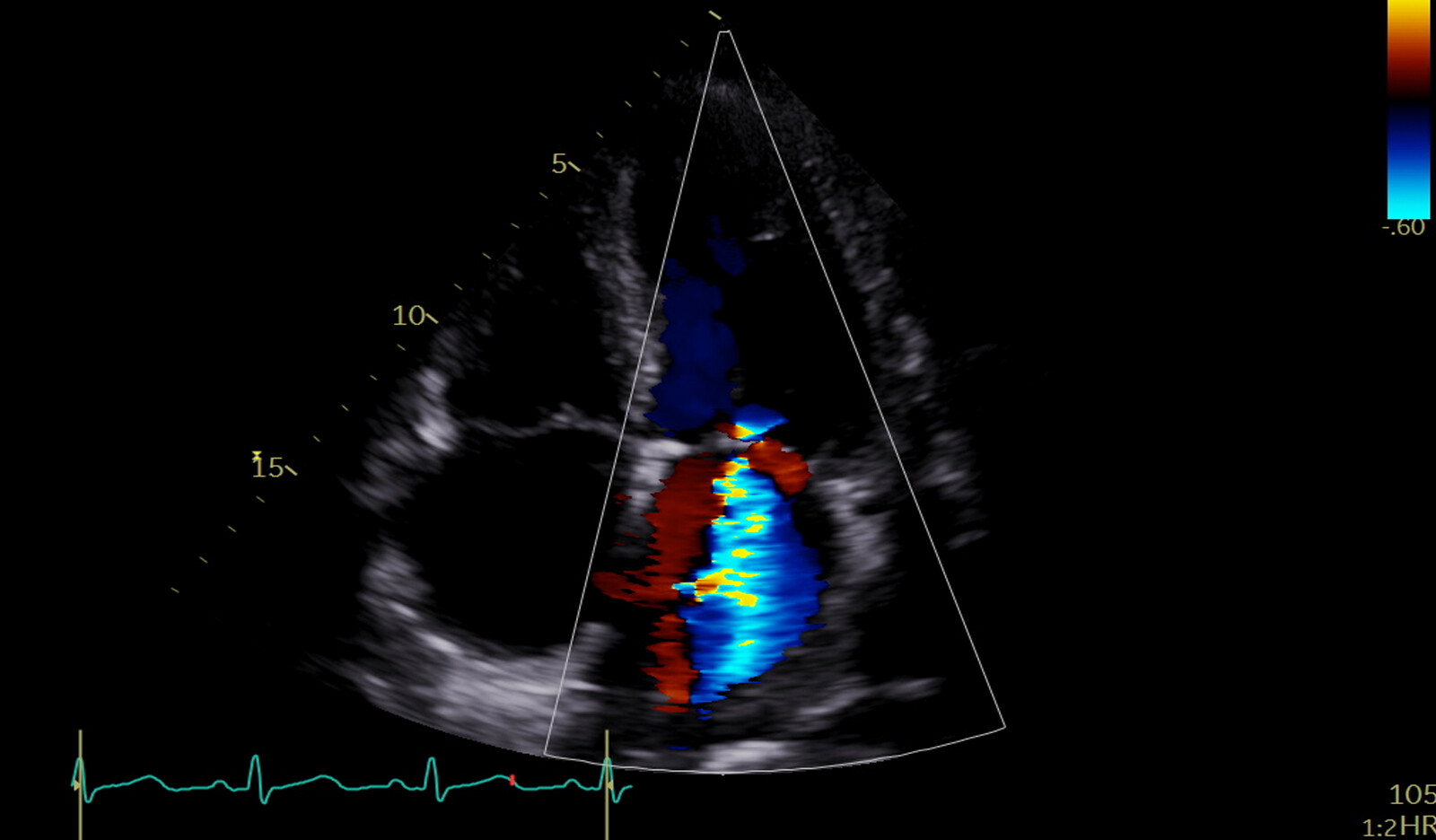
Doppler echocardiography assessment of RVol by flow convergence, also called the proximal isovelocity surface area (PISA) method, is a key step for assessment of severity of MR.
Other quantitative volumetric methods have been proposed for determining RVol as the difference between left ventricle (LV) total stroke volume (LV end-diastolic–LV end-systolic volume) and aortic forward stroke volume by TTE or cardiac magnetic resonance imaging (CMR).
However, significant discrepancies have been observed between PISA RVol and CMR-RVol in primary MR patients. PISA seems to overestimate RVol compared with the CMR volumetric method.
Therefore, the goal of this study was to:
- Compare mitral RVol determined with the PISA and with volumetric methods (TTE, CMR)
- Identify factors independently associated with the magnitude of the difference between RVol estimated by PISA and volumetric methods, respectively
- Investigate the relationship between RVol obtained with either the PISA or volumetric methods and LV size
METHODS
Study Population
This prospective study was conducted among patients referred to two heart valve centers for evaluation of primary MR.
Inclusion criteria included:
- Age 18 years or older
- Significant (moderate to severe or severe according to current guidelines)
- Chronic primary MR due to prolapse in sinus rhythm
- CMR and TTE assessment
Exclusion criteria included:
- MR from an etiology other than mitral valve prolapse
- More than mild aortic stenosis
- Aortic regurgitation, or mitral stenosis
- Presence of a prosthetic valve or an intracardiac shunt
- Standard contraindication for CMR
- Atrial fibrillation
- Poor TTE image quality
- Refusal to participate in the study
Echocardiography
All patients underwent a comprehensive Doppler transthoracic echocardiography (TTE) study performed by experienced echocardiographers blinded to CMR data using commercially available ultrasound systems.
MR severity was graded according to an integrative multiparametric approach. The vena contracta (VC) width was obtained in a magnified view of the parasternal long-axis or apical three chamber view in which the proximal jet size was the largest. The VC width was then measured as the narrowest portion of the mitral regurgitant jet. The PISA radius was measured in midsystole, on either the apical or parasternal view, as appropriate, with the lower Nyquist limit set to aliasing velocity between 30 and 40 cm/sec and magnified in the area of flow convergence. The peak MR jet velocity and velocity-time integral were determined using continuous-wave Doppler across the mitral valve.
The MR effective regurgitant orifice area (MR-EROA) was calculated using the PISA radius, peak MR velocity, and aliasing velocity. The PISA geometric convergence angle (a°) was determined to be the minimum angle between two sides of the proximal flow convergence field. Based on the observed a°, an angle-corrected PISA-RVol was calculated for all patients as follows: PISA-RVol_angle = PISARVol x (a°/180°).
Left ventricular (LV) volumes and ejection fraction (LVEF) were measured according to Simpson’s biplane method. Left ventricular forward stroke volume was calculated as the product of the LV outflow tract velocity-time integral and the LV outflow tract cross-sectional area. Mitral RVol by the TTE volumetric method (TTE-RVol) was calculated by subtracting the LV forward stroke volume from the total LV stroke volume obtained by Simpson’s method.
Transthoracic echocardiographic regurgitant fraction (TTE-RF) was defined as TTE-RVol divided by LV total stroke volume, expressed as a percentage.
Cardiac Magnetic Resonance Imaging
Cardiac magnetic resonance imaging studies were performed by operators blinded to the patient’s echocardiographic data. Assessment of LV function was performed with a cine steady-state free precession pulse sequence, with retrospective gating, in end expiration breath hold.
The following projections were acquired: two-chamber, four-chamber, and parallel contiguous short axis (to cover the entire LV from the mitral plane to the apex). End diastolic and end-systolic areas were manually delineated in all slices acquired in the short-axis view for each ventricle, allowing for the assessment of end-diastolic and end-systolic volumes and the calculation of the LVEF (CMR-LVEF). Left ventricular end-diastolic volume (LVEDV; CMR-LVEDV) and end-systolic volume (CMR-LVESV) were calculated using manual contouring, including trabeculations and papillary muscle as part of the volume.
RESULTS
188 patients included in the study; 48 women [26%]; median age, 66 years [57-73].
The distribution of time between TTE and CMR studies was as follows: performed the same day, 64%; between 1 and 30 days, 23%; between 30 and 90 days, 13%.
A weak correlation was observed between PISA-RVol and CMR-RVol (Y = 0.35X + 36, r = 0.29, P < .001). Replacing PISA-RVol by PISARVol_angle did not improve the correlation with CMR-RVol (r = 0.23, P = .001). Using the Bland-Altman method, the mean difference in RVol (PISA-RVol–CMR-RVol) was 8 mL with wide limits of agreement (–45; 61 mL).
There was a significant proportional bias between PISA-RVol and CMR-RVol. CMR-RVol and TTE-RVol were moderately correlated (r = 0.55, P<.001). When considering the currently recommended threshold of mitral RVol of > 60mL to define severe MR, 67 patients (36% of the study population) would be reclassified from severe using PISA-RVol to moderate MR using TTE-RVol, and 60 patients (32% of the study population) would be reclassified from severe using PISARVol to moderate MR using CMR-RVol.
The authors presented further analysis – they performed linear regression analyses to identify characteristics associated with the magnitude of the difference between RVol assessed by PISA versus either CMR or TTE volumetric methods (∆[PISA-CMR]RVol and ∆[PISA-TTE]RVol, respectively).
CONCLUSION
The author concluded that in this study, that was based on a ‘‘real-world’’ cohort of patients with chronic significant primary MR due to valve prolapse, showed that mitral RVol values estimated by TTE and CMR are not directly comparable.
They further commented that the expected proportional relationship between RVol obtained using volumetric methods and LV size, which was unexpectedly not observed with RVol-PISA, suggests that PISA-RVol would be inaccurate.
Given that RVol values obtained by volumetric methods are highly dependent on LV size, determination of a unique RVol threshold for severe MR is challenging. In contrast to RVol, calculating RF by volumetric methods allows the quantification of MR severity independently from LV size.
 Español
Español
 English
English